Q. What is Hyponatraemia?
A . When people have low sodium levels in their blood the condition is called Hyponatraemia. Sodium is one of a number of electrolytes essential for many body functions. Hyponatraemia is the most common form of electrolyte abnormality. It can be a feature of many conditions (e.g. liver or kidney failure) or result from drug treatments (e.g. some anti-hypertensives or some anti-epleptics). In many cases, particularly if the sodium level is close to normal it may lead to no symptoms. However severe cases, if not identified or adequately treated, can cause coma and can be fatal. Children and older people are most at risk.
The specific form of hyponatraemia that occurred in the cases of the children examined by the inquiry – dilutional hyponatraemia – relates to fluid intake that does not contain sufficient sodium to maintain normal sodium levels.
Q. Why was the Inquiry set up and what did it find?
A. The Inquiry into Hyponatraemia Related Deaths (IHRD) was set up to investigate the deaths of five children in hospitals in Northern Ireland. It published its findings on 31 January 2018.
It found that some of the five deaths were avoidable. It also concluded that the culture of the health service at the time, the arrangements in place to ensure the quality of services and the behaviour of individuals had all contributed to those unnecessary deaths.
The report sets out 96 recommendations across 10 themes where Mr Justice O’Hara identified failings in -
- competency in fluid management;
- honesty in reporting;
- professionalism in investigation
- focus in leadership;
- and respect for parental involvement
The report can be accessed here: http://www.ihrdni.org/inquiry-report.htm
Q. How can you be sure that this isn’t just another report that sits on a shelf?
A. The Department has established a comprehensive programme to take forward implementation of the recommendations. The programme includes a number of members:
Q. How has the Department of Health responded?
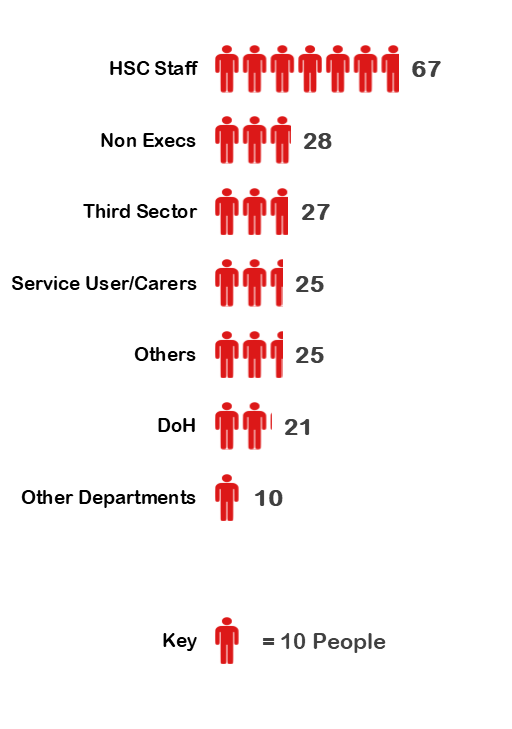
A. We have gathered together more than 200 people from different backgrounds to work through how best to implement the recommendations.
They include service users and carers, representatives of the voluntary and community sector, people from health and social care organisations, non-executive directors of health and social care organisations, and department staff. Every one of them brings a unique perspective, expertise and personal experience. This new way of working will help ensure that our response to the report is robust and effective.
Q. The report calls for a statutory Duty of Candour. What does that mean?
A. A Duty of Candour would create a legal responsibility for all healthcare organisations and individual staff to be honest when things go wrong. This duty would not just apply to being open and honest with patients but also on the need to be open and honest within organisations in reporting adverse incidents or near misses that may have led to harm.
The Duty of Candour Workstream and Being Open sub-group has prepared a list of Frequently Asked Questions (FAQ’s) to support understanding on how this work will be taken forward. The Being open and Duty of Candour FAQ’s may be accessed here.
Q. Why are we including service users and carers, the Third Sector and others?
A. How we go about making change is just as important as the changes themselves. We need the expertise and experience of others if we are to get this right and service users and carers are integral to this process. They are experts through experience and will help ensure that the changes we make work in practice.
Q. How can I get involved?
A. We want to ensure that everyone has a chance to have their say. An Involvement Strategy has been developed to help shape how people and organisations from across Northern Ireland are involved in the programme of work. We will engage with people in a range of different ways including via technology to enable people to participate no matter where they live.
If you want to take part please register your interest Here
Or Email us at ihrd.implementation@health-ni.gov.uk
Q. But doesn’t this just affect children or those with Hyponatraemia?
A. Many of the recommendations are specific to children, however the report has much wider implications. It raises many issues –
- how the health service works;
- what patients and their loved ones are told when they are ill;
- what happens when things go badly;
- And how we improve safeguards for all
We expect the health service to be open about everyone’s care. That is why it is important that as many people as possible are involved in ensuring that implementation works.
Q. What difference will it make?
- Greater openness and transparency with patients;
- Help prevent problems which can lead to a lack of trust and the breakdown of relationships between service providers and service users and carers in the first place;
- It will change the way we deliver health and social care services;
Q. How long will it take?
A. We expect the vast majority of recommendations to be implemented by mid 2020. There are a small number, including the creation of an Independent Medical Examiner and the introduction of a statutory Duty of Candour that will require an Executive and Assembly to put through legislation.
Q. How can so much be done without an Executive and Assembly?
A. The vast majority of the recommendations are in relation to how we work and do not require Ministerial approval. In the other cases we will do all the background work so that decisions can be made by an incoming Minister as quickly as possible.
Q. Why does it take so much time?
A. This is a major piece of work with implications for the entire health and social care system. The 96 recommendations will need 120 actions to be implemented. It is important that all are implemented in the way intended by the Inquiry and that they make services safer. This involves engaging with all stakeholders including patients, families and members of the general public. Designing the new system together will make sure that we get it right.
Q. Will those at fault be held accountable?
A. The purpose of the programme is to address the report’s recommendations. Separate to this there are a range of investigations on-going; by employers, professional regulators, the PSNI and the Coroner. They will reach their respective conclusions and determine a course of action in due course.
Q. Will there be updates on progress?
A. There will be regular updates on our work which can be accessed Here. They will also be emailed to those registering their interest through the site.
